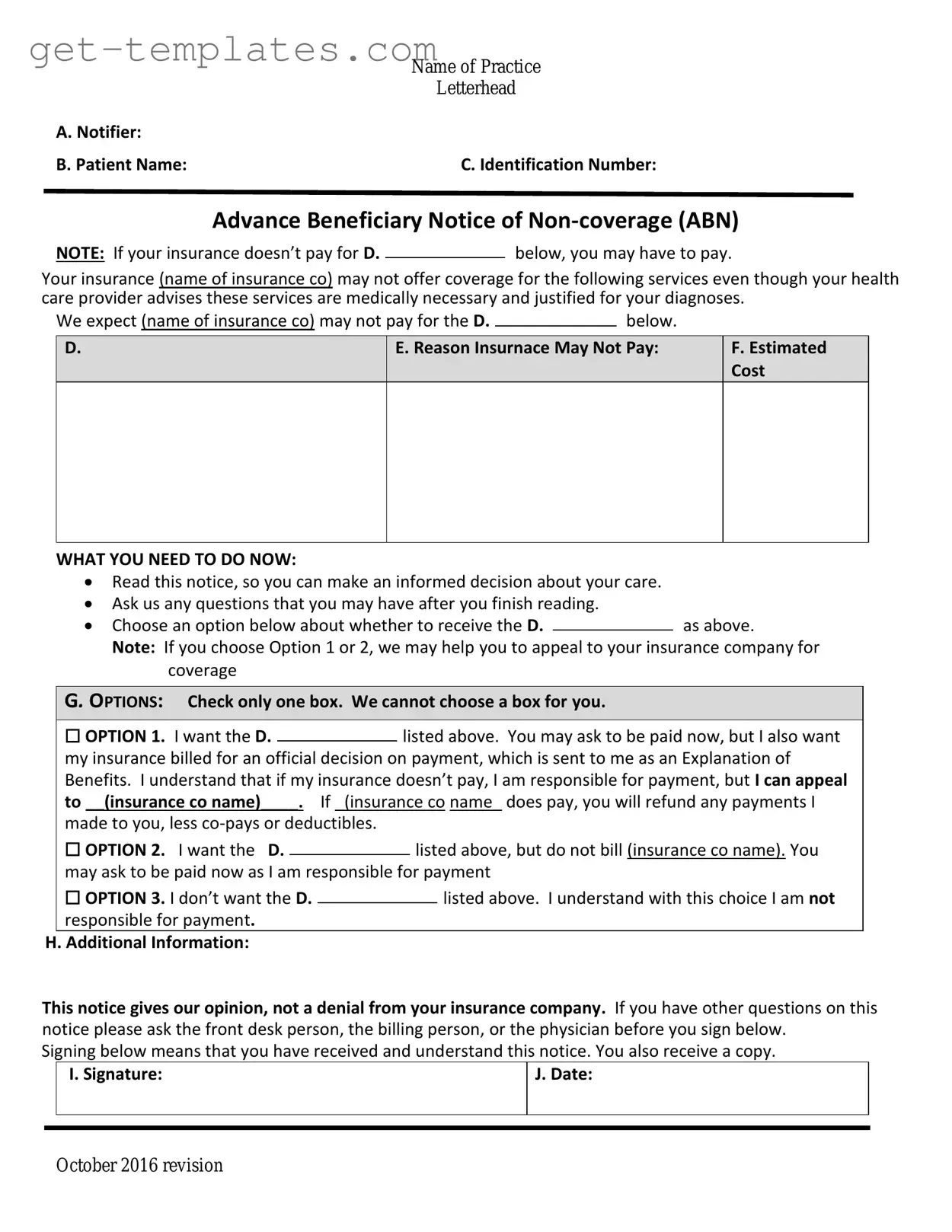
Fill in a Valid Advance Beneficiary Notice of Non-coverage Template
The Advance Beneficiary Notice of Non-coverage (ABN) is a crucial document that informs Medicare beneficiaries when a service or item may not be covered by Medicare. This form empowers patients to make informed decisions about their healthcare by clearly outlining potential out-of-pocket costs. Understanding the ABN can help beneficiaries navigate their options and avoid unexpected expenses.
Get Document Online
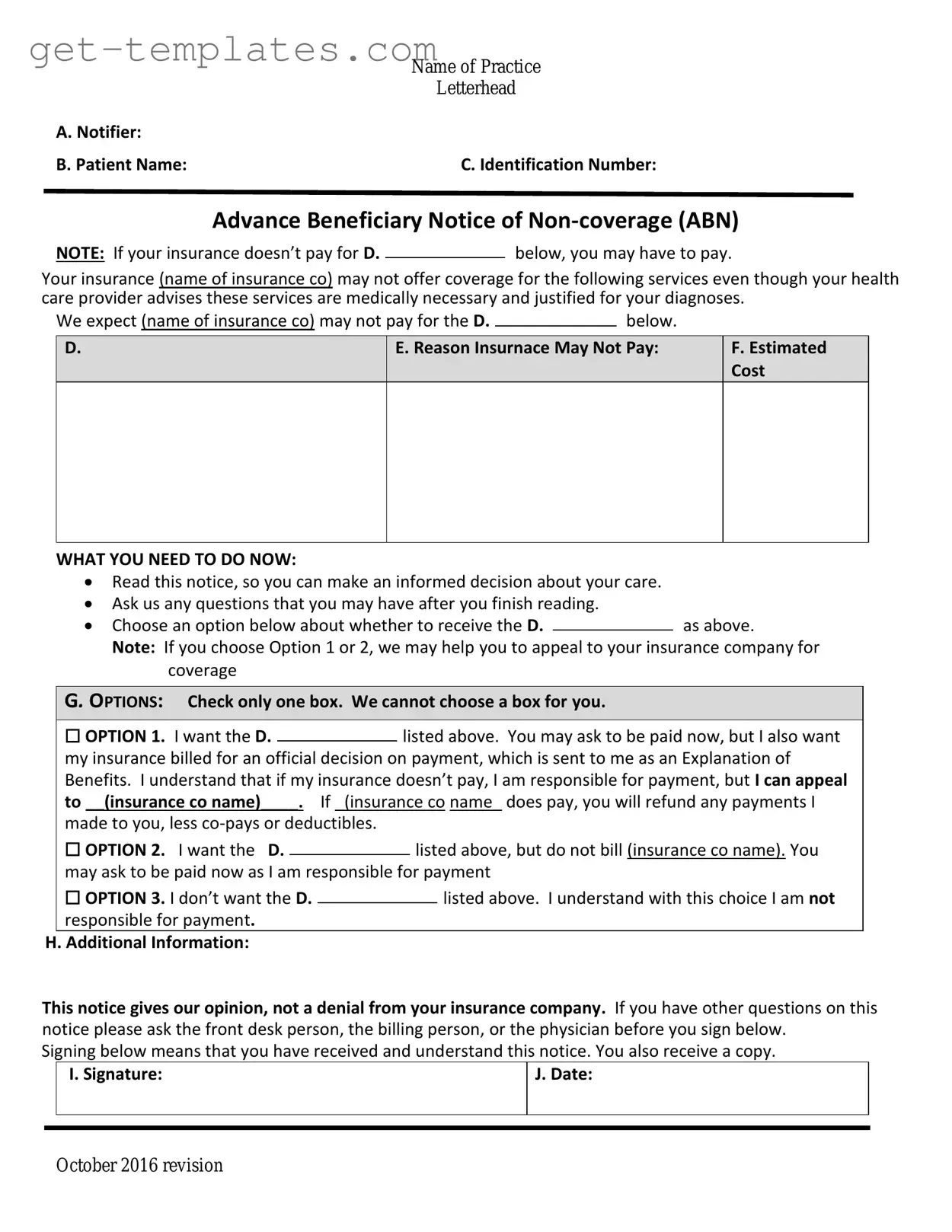
Fill in a Valid Advance Beneficiary Notice of Non-coverage Template
Get Document Online
You’re halfway through — finish the form
Finish Advance Beneficiary Notice of Non-coverage online — edit, save, download made easy.
Get Document Online
or
⇓ PDF Form