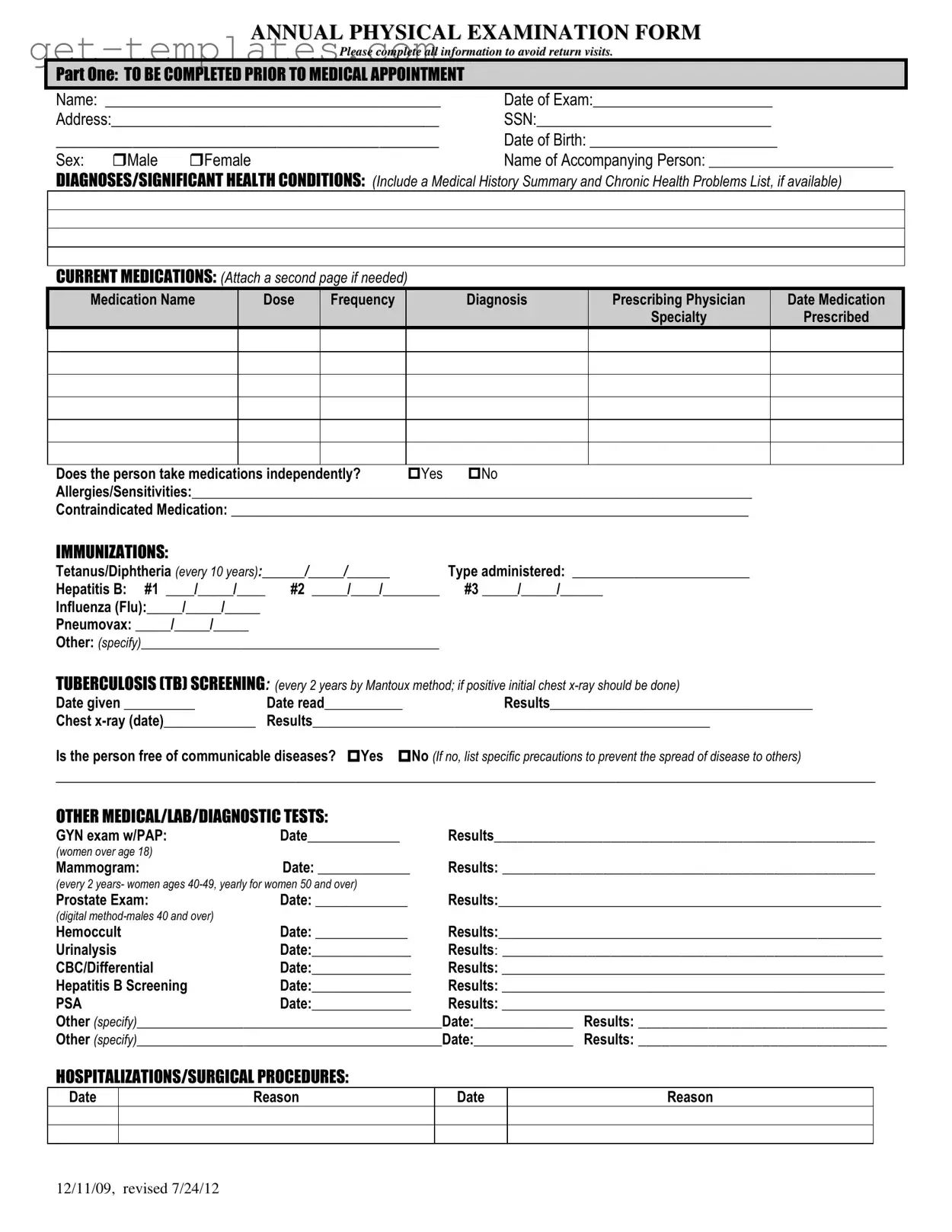
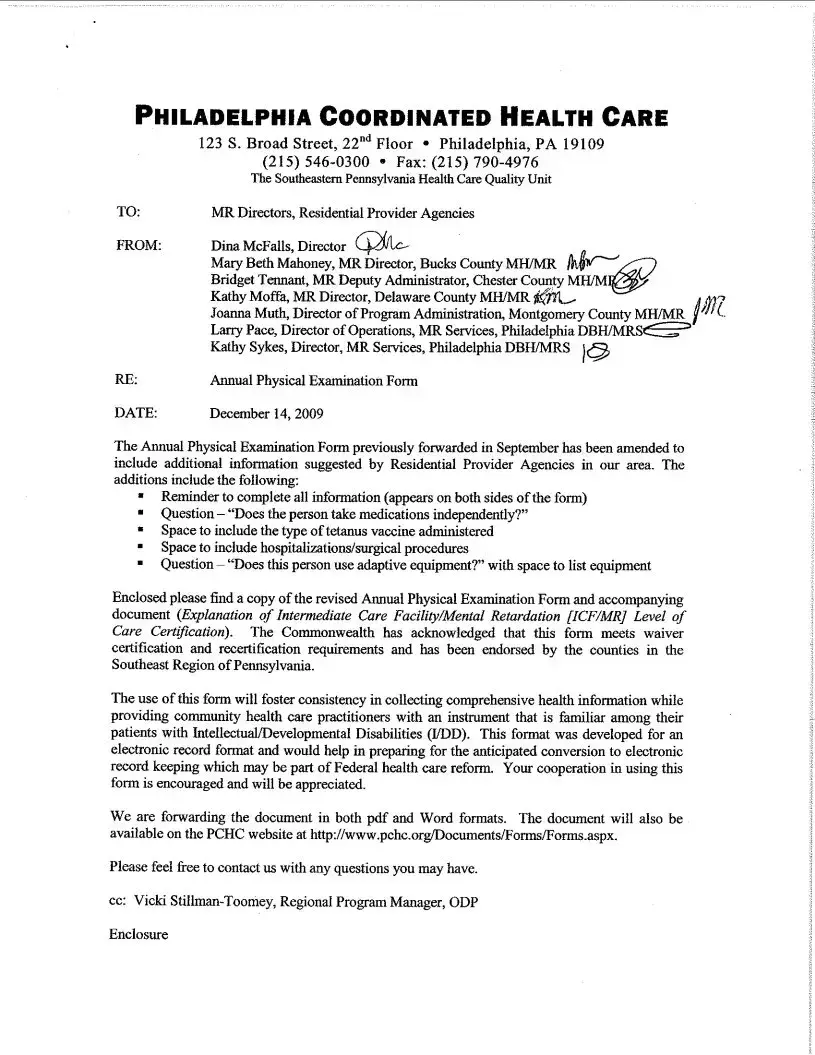
The Annual Physical Examination form is designed to gather essential health information before your medical appointment. It helps healthcare providers assess your overall health, identify any significant medical conditions, and recommend necessary tests or treatments.
Part One requires personal details such as your name, date of exam, address, Social Security Number, date of birth, and sex. You must also provide information about any significant health conditions, current medications, allergies, and immunizations. This section ensures that your healthcare provider has a comprehensive view of your health history.
How should I list my current medications?
List each medication by name, dosage, frequency, diagnosis, prescribing physician, and the date it was prescribed. If you take multiple medications, you may attach a second page. Indicate whether you take medications independently or need assistance.
What should I do if I have allergies or sensitivities?
Clearly list any allergies or sensitivities in the designated section of the form. This information is crucial for your healthcare provider to avoid prescribing medications that could cause adverse reactions.
How often should I update my immunization records?
Immunization records should be updated regularly. For example, the Tetanus/Diphtheria vaccine is required every 10 years, while the Influenza vaccine is recommended annually. Keep track of all immunizations and provide the dates administered on the form.
What if I have a history of communicable diseases?
If you have a history of communicable diseases, indicate this on the form. You should also list any specific precautions you take to prevent spreading the disease to others. This information is vital for ensuring the safety of both you and other patients.
What types of tests are included in the general physical examination?
The general physical examination includes evaluations of vital signs such as blood pressure, pulse, and temperature. It also assesses various body systems, including eyes, ears, lungs, and cardiovascular health. Results from any additional tests, like blood work or imaging, should also be documented.
How should I handle a change in health status?
If you experience a change in health status since your last visit, you must specify this on the form. This could include new symptoms, diagnoses, or treatments. Keeping your healthcare provider informed allows for better management of your health.
What recommendations might I receive after my examination?
After your examination, you may receive recommendations for health maintenance. This could include suggestions for lab work, therapies, exercise, dietary changes, and frequency of screenings. These recommendations aim to enhance your overall health and prevent future issues.
What happens if I need further evaluation by a specialist?
If your healthcare provider recommends further evaluation by a specialist, this will be noted on the form. Follow-up appointments may be necessary to address specific health concerns or conditions identified during your examination.