Fill in a Valid Tb Test Template
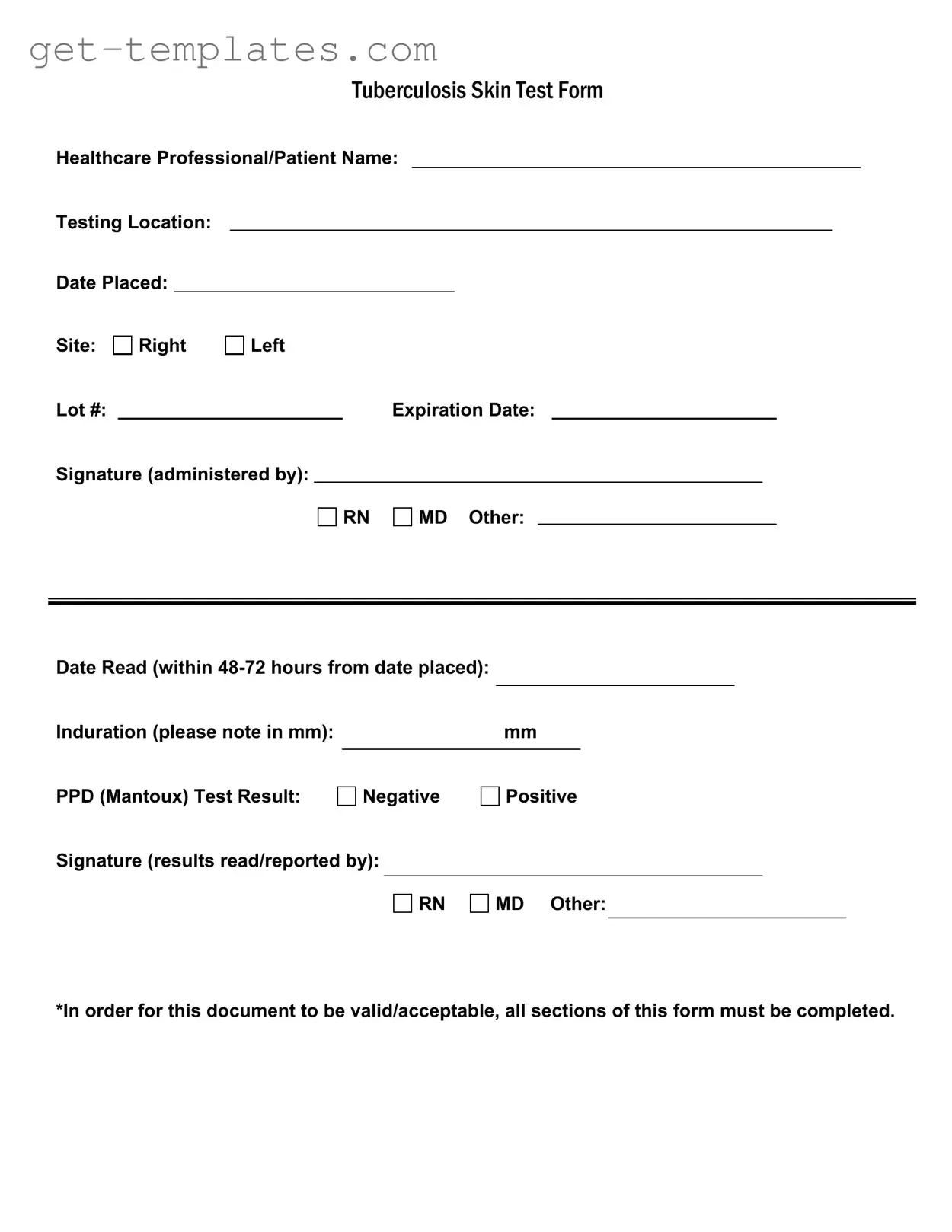
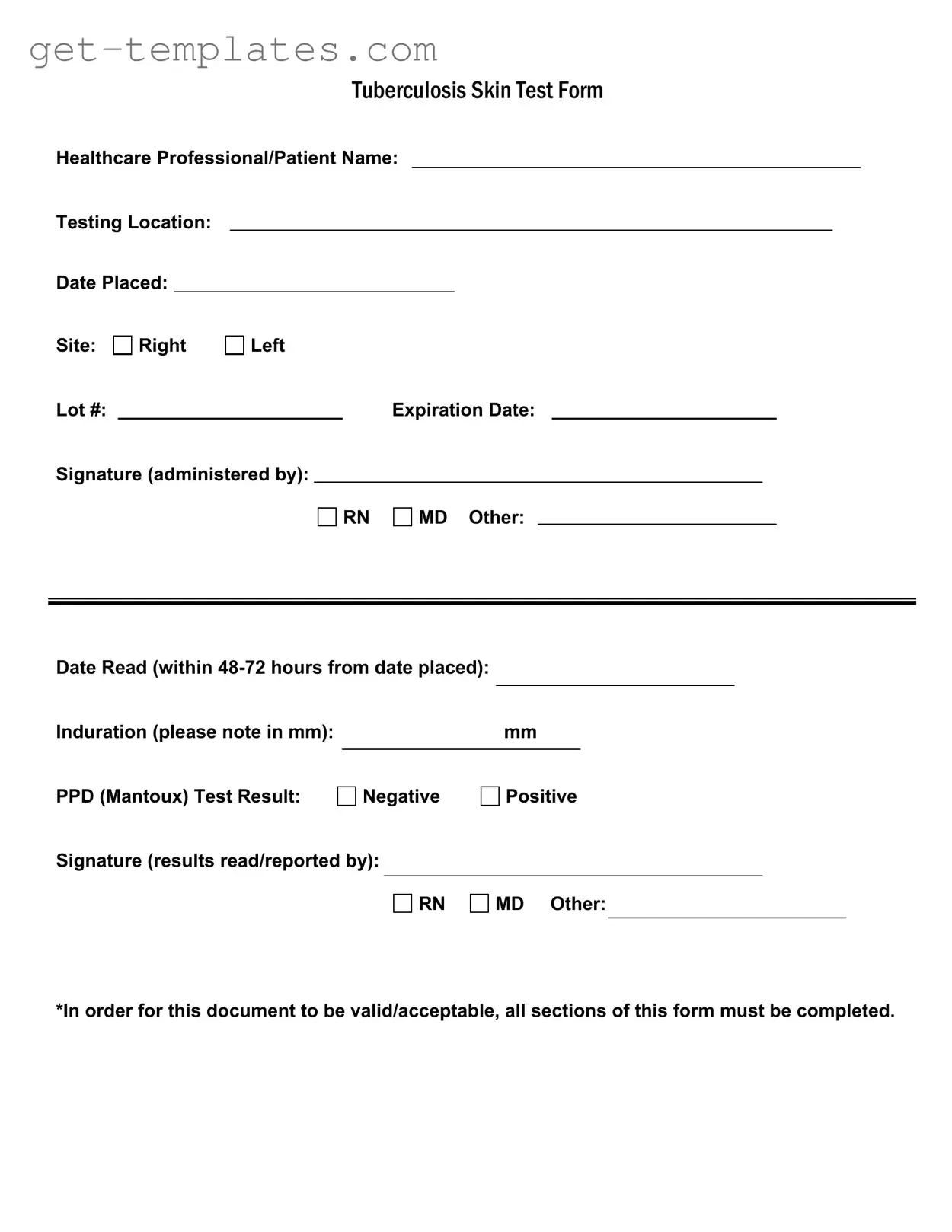
The Tuberculosis Skin Test Form is a critical document used to record the details of a tuberculosis (TB) skin test, commonly known as the PPD (Mantoux) test. This form captures essential information such as the healthcare professional's name, testing location, and test results. Completing all sections of this form is necessary for it to be valid and acceptable.
Get Document Online
Fill in a Valid Tb Test Template
Get Document Online
You’re halfway through — finish the form
Finish Tb Test online — edit, save, download made easy.
Get Document Online
or
⇓ PDF Form